Rethinking Resistance:
New Life for a “Last Resort” Antibiotic
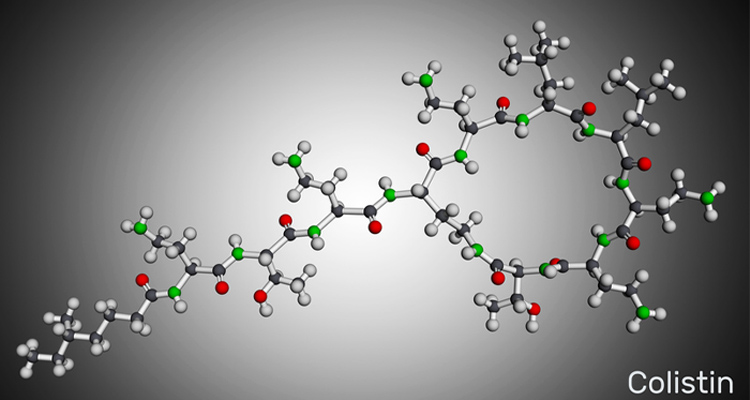
The antibiotic colistin remains effective against some antibiotic-resistant bacteria when tested in conditions that mimic the human body. Photo credit: iStock/Bacsica.
A new study offers fresh hope in the fight against deadly, drug-resistant infections.
Researchers from University of California San Diego and The University of Texas at Tyler have discovered that colistin, an antibiotic often regarded as a “last resort” treatment for multi-drug resistant infections, remains effective against a dangerous class of antibiotic-resistant bacteria when tested in conditions that better mimic the human body. The research is published in the June 16 edition of The Journal of Clinical Investigation.
Globally there are increasing reports of bacteria carrying the mobilized colistin resistance (mcr) gene—an alarming, mobile form of resistance that can rapidly spread among bacteria. The presence of the mcr gene renders many important Gram-negative pathogens, like E. coli and Klebsiella pneumoniae, resistant to colistin in the standard lab testing protocols performed in test tubes and petri dishes. Consequently, colistin is typically ruled out as a treatment option for patients with lung, bloodstream, or urinary tract infections once mcr is detected.
However, this new research published by an interdisciplinary team, suggests standard testing methods may be missing the full picture.
“When we tested colistin in lab conditions that resemble the human body—including the presence of bicarbonate and components of the immune system—it was surprisingly effective against mcr-expressing bacteria,” said Monika Kumaraswamy, M.D., lead author and chief of infectious diseases at UT Health East Texas and associate professor of medicine at the UT Tyler School of Medicine. “This work flips the narrative about colistin and clinical antimicrobial susceptibility testing. It’s not that the drug is necessarily obsolete against mcr-positive bacteria—it’s that our testing methods have been incomplete.”
The research findings show colistin kills mcr-positive bacteria in human blood, enhances bacterial clearance by our immune cells, and improves survival in infected mice—all at drug concentrations achievable with standard dosing.
“These results don’t mean we should throw out current guidelines,” added senior author Victor Nizet M.D., distinguished professor of pediatrics at UC San Diego School of Medicine and professor of pharmacy at UC San Diego Skaggs School of Pharmacy and Pharmaceutical Sciences. “But they do underscore the need to modernize antimicrobial susceptibility testing. Standard lab tests don’t account for the synergy between drugs and our immune system. This can make us underestimate a drug’s true potential.”
Colistin was developed in the 1950s but by the 1970s, many doctors stopped using it due to the risks associated with its side effects and the rise of newer safer antibiotics. In recent years, its clinical use has resurged as a last-ditch option against extensively drug-resistant bacteria. However, the global rise of plasmid-borne mcr genes has raised fears that even this last-line therapy could soon be rendered ineffective.
The researchers are calling for changes in how antibiotics are tested in the clinical microbiology laboratory—using conditions that more closely resemble the human body, including elements of the immune system. These changes could help uncover the hidden potential of existing antibiotics once thought to be ineffective and lead to new treatment options in the battle against antimicrobial resistance.
— Joyce Pritchett
Communications Specialist, UC San Diego School of Medicine
